By Kosali Simon
Highlights from Dr. Jay Bhattacharya’s remarks at the 2026 AEA Meetings
At the 2026 AEA Meetings, NIH Director Dr. Jay Bhattacharya delivered a clear message to economists: NIH is eager to engage health economics and interdisciplinary teams to achieve its mission of advancing knowledge to improve health and longevity. He argued that stagnant US life expectancy, rising chronic disease burden, and unsustainable health spending cannot be solved by biomedical science alone. Health economics, he emphasized, must be a full partner.
Dr. Bhattacharya announced a major shift in NIH policy. He described prior restrictions that narrowed the scope of economics research eligible for NIH funding that are now removed. Going forward, health economics proposals will be evaluated like any other science at NIH, based on rigor, relevance to health, and potential for impact.
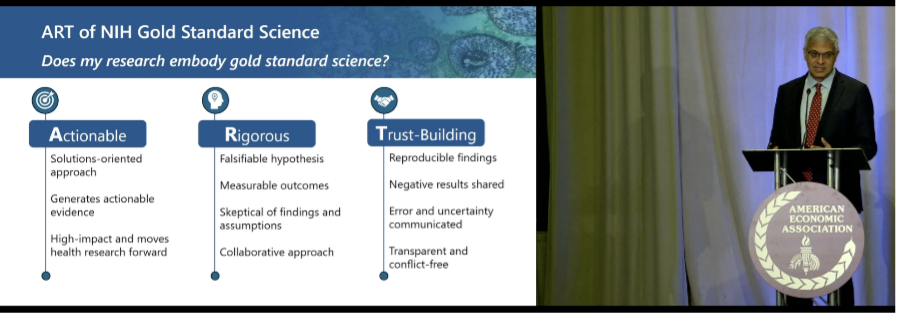
He encouraged economists to submit work that is actionable, reproducible, and testable (ART), particularly research that informs financing, incentives, workforce challenges, consumer decision making, and efficiency in care delivery. His message was both an invitation and a challenge: if economists want to shape the future of population health, NIH is now explicitly asking them to apply, and, to be involved in the review process. In his own words, “Biomedical discovery alone has not delivered population health gains. Economics is essential if we want longer, healthier lives”.
More details
1. Goals as NIH Director
Dr. Bhattacharya framed his remarks around five goals for his tenure as NIH Director, focusing this talk on one priority: improving population health. He argued that despite decades of scientific breakthroughs, the US has failed to deliver sustained improvements in life expectancy or quality of life. Health economics, he said, is indispensable to understanding why. NIH is repositioning health economics from a peripheral or constrained activity to a core component of its mission.
2. The problem: health outcomes, productivity, and costs
Dr. Bhattacharya highlighted several trends motivating the policy change:
- US life expectancy has stagnated since about 2010, with COVID producing a sharp decline and only partial recovery.
- Chronic diseases such as diabetes, obesity, and Alzheimer-related dementias continue to expand, driving morbidity and long-term costs.
- Research productivity appears to be slowing, with greater investment yielding smaller marginal gains.
- Health spending continues to rise toward 20 percent of GDP without commensurate improvements in outcomes.
Together, these patterns suggest a system that generates innovation but struggles to translate it into broad, sustained health gains.
3. NIH’s track record with economics
He emphasized that NIH already has a strong legacy of enabling economics research. He cited long-standing investments such as the Health and Retirement Study, SEER cancer registries, and Alzheimer’s research infrastructure, which have supported decades of influential economic and policy analysis. Economists have already shown their value within NIH-supported ecosystems, and expanding this role is both logical and necessary.
4. The policy shift: removing limits on health economics
The centerpiece of the talk was to announce that NIH will remove prior limits that constrained health economics research.
- Economics and health economics proposals will be judged under the same standards as other sciences.
- There are no blanket topic exclusions, provided the work advances NIH’s mission to improve length and quality of life.
- Relevance to health outcomes must be explicit, but the pathway can be policy, delivery, financing, or behavior.
This was framed as a correction to earlier guidance that had unintentionally narrowed the scope of valuable research. According to Dr. Bhattacharya, “If the work advances health and is scientifically rigorous, it belongs at NIH”.
5. What NIH wants to fund: ART expectations and standards
Dr. Bhattacharya outlined what successful NIH-funded health economics should look like. He emphasized three core attributes:
- Actionable: Research should inform decisions, interventions, or policy design, not just describe problems
- Reproducible: Clear hypotheses, transparent methods, data sharing, and openness to null results are essential
- Testable: NIH favors work that generates falsifiable claims and evidence that can be validated or challenged.
He also stressed interdisciplinary collaboration when appropriate, particularly with clinicians, biomedical scientists, and public health researchers.
6. Illustrative priority areas
He offered examples of economic research domains that naturally align with NIH priorities:
- Financing and incentive design in health care
- Health care workforce supply, demand, and organization
- Consumer decision making and behavioral responses
- Cost, efficiency, and delivery system design
- Economic burden and value assessment for chronic and aging-related diseases
These examples were explicitly described as illustrative, not restrictive.
7. A direct call to economists
Dr. Bhattacharya closed with an unambiguous invitation. Economists, he said, should view NIH as a serious home for investigator-initiated health economics research. Addressing the chronic disease crisis and fiscal pressures in health care will require economists working alongside biomedical and clinical scientists. He emphasized that NIH is not seeking advocacy, but rigorous science that can inform real-world decisions.
What this means for ASHEcon researchers
- NIH should now be considered a viable funding destination for work that links economic mechanisms to health outcomes. Successful proposals will clearly articulate health relevance, prioritize reproducibility, and aim for actionable insights
- Projects that integrate economics with clinical, biomedical, or implementation expertise are likely to be especially competitive
- This shift signals a broader recognition that improving population health requires not just new treatments, but better incentives, delivery systems, and decision environments
